Overview
 Morton’s neuroma is a swollen or thickened nerve in the ball of your foot. When your toes are squeezed together too often and for too long, the nerve that runs between your toes can swell and get thicker. This swelling can make it painful when you walk on that foot. High-heeled, tight, or narrow shoes can make pain worse. Sometimes, changing to shoes that give your toes more room can help.
Morton’s neuroma is a swollen or thickened nerve in the ball of your foot. When your toes are squeezed together too often and for too long, the nerve that runs between your toes can swell and get thicker. This swelling can make it painful when you walk on that foot. High-heeled, tight, or narrow shoes can make pain worse. Sometimes, changing to shoes that give your toes more room can help.
Causes
A Morton’s Neuroma is not a true neuroma, which is a tumor that is generally benign. Rather, it is an enlargement of the nerve where it goes between the metatarsal bones of the foot. Because the nerve no longer fits between the gap, the pressure causes pain and sometimes numbness. This enlargement of the nerve is often an inflammation due to irritation. If the forefoot becomes compressed due to shoes that are too narrow, the nerve becomes damaged and inflamed. This inflammation means the nerve no longer fits in the space between the bones, creating further irritation and more inflammation. If this vicious circle can be broken, the problem may be resolved. However, in some situations the nerve can have fibrous tissues formed around it, which may require the destruction of the nerve or surgical removal.
Symptoms
You may initially experience a tingling sensation in the space between your toes, which gets worse over time. This leads to cramp in your toes and a sharp shooting or burning pain on the ball of your foot or at the base of your toes. The pain is often worse when walking or wearing shoes that press on the affected area. This is caused by irritation of the nerve between your toe bones (metatarsal bones). The tingling will eventually lead to pain, which can get worse over time. You may also experience cramping of your toes. The pain is usually felt as a sharp shooting or burning pain on the ball of the foot or at the base of the toes, which is often made worse when you’re walking. Some people with Morton’s neuroma feel anxious about walking or even placing their foot on the ground. The pain is likely to be more intense if you wear tight shoes, so wearing shoes that have more room in the toe area can help. Rubbing your foot may also lessen the pain.
Diagnosis
Patients with classic Morton?s neuroma symptoms will have pain with pressure at the base of the involved toes (either between the 2nd and 3rd toes, or between the 3rd and 4th toes). In addition, squeezing the front of the foot together can exacerbate symptoms. As well, they may have numbness on the sides of one toe and the adjacent toe as this corresponds with the distribution of the involved nerve.
Non Surgical Treatment
The first line of treatment is to try modifying footwear. Often simply wearing broader fitting shoes can reduce pressure on the neuroma and so reduce pain. Orthotic inserts can also help as they can again help reduce pressure on certain parts of the foot. Padding and taping the toe area is another option. In some cases a steroid injection into the foot may be suggested. This can be done as a day case without the need for anaesthesia and helps reduce inflation of the nerve. It can halt the pain in round 70 % of cases. Sometimes a combination of alcohol and local anaesthesia may be injected as this helps reduce pain.
Surgical Treatment
Surgery for Morton’s neuroma is usually a treatment of last resort. It may be recommended if you have severe pain in your foot or if non-surgical treatments haven’t worked. Surgery is usually carried out under local anaesthetic, on an outpatient basis, which means you won’t need to stay in hospital overnight. The operation can take up to 30 minutes. The surgeon will make a small incision, either on the top of your foot or on the sole. They may try to increase the space around the nerve (nerve decompression) by removing some of the surrounding tissue, or they may remove the nerve completely (nerve resection). If the nerve is removed, the area between your toes may be permanently numb. After the procedure you’ll need to wear a special protective shoe until the affected area has healed sufficiently to wear normal footwear. It can take up to four weeks to make a full recovery. Most people (about 75%) who have surgery to treat Morton’s neuroma have positive results and their painful symptoms are relieved.





 Overview
Overview Symptoms
Symptoms Overview
Overview Symptoms
Symptoms Prevention
Prevention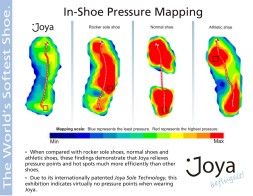



You must be logged in to post a comment.